Understanding TMJ Disorder
TMJ disorder describes problems affecting the jaw joint and the muscles that move it. It can cause jaw pain, clicking or popping sounds, stiffness, and limited opening. Symptoms often flare with chewing, yawning, or stress. Most cases are managed with simple, noninvasive care.
Your jaw clicks when you bite an apple. The condition can involve the joint disc, nearby ligaments, and chewing muscles, and pain often comes from more than one of these tissues [1]. Clenching or night grinding can overload the system; past injury, posture, and stress can add to the strain. If grinding is part of your pattern, see how night guards may reduce tooth wear and muscle load. TMJ disorder is common worldwide across teens and adults [2].
- Jaw pain near the ear or cheeks
- Clicking, popping, or grating sounds
- Limited or uneven mouth opening
- Morning jaw stiffness or tooth sensitivity
- Headaches or face aches that worsen with chewing
Diagnosis starts with your history and an exam of jaw motion, bite, and muscles. Many people improve with education, jaw rest, a softer diet for a time, guided exercises, and a well-made splint, which can reduce pain and modify joint loading in some patients [3]. Certain physical therapy methods, such as dry needling, may help select patients when used thoughtfully with other care [4]. Because headaches often overlap with jaw pain, coordinated evaluation helps identify the main source and guide treatment [5].
Early attention to habits, pain triggers, and range of motion usually makes care simpler. If you need scheduling details, our current hours are kept up to date. Joint care between dental and medical teams helps sustain long-term wellness.
Common TMJ Disorder Symptoms
TMJ disorder often shows up as pain around the jaw joint, tired chewing muscles, or joint noises. People may notice the jaw catching, shifting to one side on opening, or feeling “out of place.” Ear-related feelings, like fullness or ringing, and pressure at the temples are also common.
After a long meeting, your temple aches and your jaw feels tired. Symptoms can concentrate in the muscles in front of the ears, the cheeks, or along the jawline. Some feel a brief lock when opening wide, then a release with a sound. Others report stiffness after yawning, a sore bite after long conversations, or a jaw that drifts to one side before it fully opens. These patterns can come and go, with flares during stress or after heavy chewing.
Ear pain without infection is a frequent complaint, as the joint sits just in front of the ear canal. Pressure changes, weather shifts, or sleeping positions may amplify discomfort. A bite that “does not feel right,” especially in the morning, can reflect overnight clenching. Because tooth pain and joint pain can overlap, comparing features helps; tooth pain often localizes to one tooth and worsens with cold or sweets, while joint-muscle pain is broader and tied to jaw use. For dental-tooth pain tips, see our overview of toothache remedies.
Tracking when symptoms start, what activities provoke them, and how long they last helps your clinician find the source. Noting jaw motion changes, sounds, and any bite shift adds useful detail. Clear documentation supports a focused exam and a plan that fits your goals. Coordinated care often leads to clearer days and calmer nights.
What Causes TMJ Disorder?
TMJ disorder arises from several factors that strain the joint, its disc, or the chewing muscles. Common drivers include persistent tooth contact during the day or sleep, joint inflammation, disc position changes, and repetitive loading from habits like long chewing sessions. Anatomy, prior injury, and systemic health can also set the stage for symptoms.
Following minor whiplash, opening wide feels tight and sore. Repeated micro‑loading from daytime jaw bracing or sleep-related tooth contact can fatigue muscles and irritate joint tissues. Across populations, awake bruxism is common, which helps explain why overuse patterns can contribute to pain and stiffness [6]. In the joint itself, the supporting ligaments may loosen, allowing the disc to shift, click, or intermittently block motion. This cycle can provoke tenderness around the ear and limit opening until tissues settle.
Inflammatory joint disease can involve the jaw, particularly in younger patients with juvenile idiopathic arthritis, where careful imaging often reveals TMJ changes [7]. Certain behaviors also matter. High-volume gum chewing, for example, has been associated with jaw symptoms in some users, likely due to repetitive muscular load [8]. Beyond the jaw, body-wide pain conditions and gut–brain interactions can heighten sensitivity, and people with irritable bowel syndrome show higher TMD prevalence in pooled data [9]. These influences do not act alone; they usually interact with personal anatomy, coping patterns, and recovery capacity.
For patients, the key is to notice patterns. Track when symptoms rise, which tasks provoke them, and what eases them. If nighttime discomfort parallels snoring or unrestful sleep, reviewing practical airway screening tools may clarify a hidden contributor. Small adjustments, paired with a focused exam, often calm irritated tissues and prevent recurrence. Timely attention to jaw habits supports steadier comfort and function.
How Jaw Pain Affects Daily Life
Jaw pain can make everyday tasks harder than they should be. Eating, speaking, and yawning may feel tiring or sharp, so people often avoid certain foods or long conversations. Sleep can be interrupted by discomfort, which leads to morning stiffness and daytime fatigue. With TMJ disorder, this strain can ripple into work, school, and social plans.
Halfway through lunch, your jaw tightens and you stop chewing on one side. Pain often triggers protective muscle guarding, which shortens opening and shifts motion to “easier” paths. That compensation can add load to other muscles, creating neck tension or temple aches. Over time, people may cut food into smaller pieces, slow their pace of eating, or limit singing and exercise that require heavy breathing through an open mouth. These small adjustments add up and can reduce confidence during meals or meetings.
Nighttime clenching can fragment sleep, so mornings start with sore muscles and a bite that feels “off.” Daytime habits, like working with the head forward or cradling a phone, may keep the jaw slightly clenched, increasing fatigue by evening. Because snoring or disrupted breathing can coexist with jaw muscle tension, learning to recognize signs of airway issues can help; see how to tell snoring from sleep apnea if sleep feels unrefreshing.
Jaw pain can also affect oral care and appointments. Brushing and flossing may feel awkward when opening is limited, and long procedures are harder to tolerate without planning breaks. Travel days, high-caffeine schedules, and tight deadlines can intensify clenching, so symptoms may spike at the worst times. Tracking triggers, comfort strategies, and the times of day your jaw feels best gives your clinician a clearer map to guide care. Early, focused care helps restore comfort and daily function.
The Connection Between Clicking Jaw and TMJ
A clicking jaw is usually related to how the temporomandibular joint moves. Most clicks happen when the joint’s soft disc slips slightly forward, then snaps back into place as you open or close. This is called disc displacement with reduction. A painless, occasional click can be harmless, but clicking with pain, locking, or limited opening may signal TMJ disorder.
During a yawn, a pop occurs and opening feels smoother. The joint’s disc cushions the lower jaw bone as it moves in the socket. If ligaments are lax or the disc sits a bit forward, the disc may recapture during motion, creating a click. A second sound on closing can occur for the same reason. When nearby tissues become irritated, clicking may come with tenderness, brief catching, or a feeling that the jaw shifts path.
Patterns matter. Repeated wide opening, one-sided chewing, or prolonged jaw bracing can make clicks more frequent by stressing the disc and supporting ligaments. Posture and muscle coordination also play roles, because the joint and chewing muscles work as a unit. If a click is new, painful, or paired with stiffness or brief “stuck” episodes, a focused exam helps distinguish joint sounds from muscle pain and guides next steps. Clear documentation of when the sound occurs, which side you feel it on, and whether motion improves after the click speeds diagnosis.
In short, the sound is a mechanical sign, not a diagnosis by itself. Understanding when and why it happens helps target simple, effective care. Addressing the cause of the click often restores smooth, quiet motion.
Exploring TMJ Treatment Options
Treatment focuses on calming irritated tissues, restoring smooth motion, and protecting the joint. Most people start with conservative care, such as habit coaching, brief rest from heavy chewing, gentle jaw exercises, and a well-fitted splint. Short courses of pain relievers, heat or ice, and targeted physical therapy can support healing. Plans are tailored to whether pain is mainly from muscles, the joint, or both.
After a tough steak, your jaw throbs near the ear. Reversible steps come first because they are safe and effective for many. A splint worn at night can reduce muscle load and shield teeth from grinding. Simple exercises improve coordination and opening without forcing the joint. Coaching often includes relaxed jaw posture, smaller bites, pacing meals, and stress strategies that reduce daytime clenching.
When the joint capsule is inflamed or motion stays limited, your dentist may discuss procedures that wash the joint or improve lubrication. Arthrocentesis or arthroscopy can release tight tissues and remove irritants in select cases. Injections are sometimes considered; for example, hyaluronic acid has reduced pain in randomized trials analyzed in a meta-analysis, though responses vary and selection matters [10]. Decisions weigh symptoms, exam findings, and your goals.
Muscle-dominant pain may benefit from manual therapy, stretching, and cueing to avoid jaw bracing during focused tasks. If headaches or neck tension overlap, coordinated care with your medical team can clarify sources and prevent flare cycles. Rarely, persistent locking or major structural changes lead to surgical options. These choices are reserved for specific diagnoses after imaging and stepwise conservative care.
TMJ disorder care works best when you track triggers, adjust routines, and follow a gradual plan. If symptoms linger, a focused evaluation helps map the right next step at the right time. Collaborative care supports durable comfort and function.
Effective TMJ Therapy Techniques
Effective therapy aims to calm pain, improve motion, and reduce overload on the jaw joint. Most people start with simple, structured steps they can practice at home, then add clinician-guided care if needed. For TMJ disorder, plans are individualized to whether symptoms arise mainly from muscles, the joint, or both.
While reading, your jaw tenses after 10 minutes. Begin with a relaxed “rest” position: lips together, teeth apart, tongue lightly on the palate. Use nasal breathing and a quiet, even pace of speech to avoid clenching. Gentle heat for 10–15 minutes softens tight muscles; a brief cold pack can settle a flare. Controlled opening with the tongue on the palate, small side-to-side glides, and light isometric holds build coordination without forcing the joint. Spread tough foods across meals, cut portions small, and pause between bites to lower peak loads.
When symptoms center in the muscles, a physical therapist can guide manual techniques and graded exercises. In people with TMD who also have chronic headaches, physiotherapy has shown benefit in systematic review, suggesting a role for targeted muscle care [11]. This approach often pairs well with cueing to unclench during focused tasks and brief posture resets through the day.
For joint-dominant pain or stiffness, minimally invasive procedures are considered after conservative steps. Arthrocentesis, which rinses the joint and releases tight tissue, has varied protocols and mixed findings across studies, so patient selection matters [12]. In osteoarthritis of the TMJ, reviews of non-surgical treatments report variable effectiveness across splints, medications, and injectables; decisions should match diagnosis and goals [13]. Autologous injections have been studied, but evidence remains heterogeneous and technique-dependent, so they are reserved for select cases [14].
Track triggers, practice your home routine, and share specific changes you notice. If progress stalls, a focused exam can refine the plan or add the right next step. Team-based planning often brings steadier relief over time.
The Role of TMJ Splints in Treatment
TMJ splints are custom, removable appliances that help reduce strain on the jaw joints and muscles. They can protect teeth from grinding, guide smoother motion, and lower pain when used as part of a conservative plan [15]. Most are worn at night; some designs are used briefly during the day if indicated.
Splints work by sharing bite forces across teeth, limiting heavy contact, and stabilizing jaw position during movement. A well-fitted stabilization splint aims for even, light contacts so muscles can relax. Anterior repositioning splints, used for specific joint conditions, temporarily guide the lower jaw slightly forward to improve how the disc and joint surfaces meet during opening. Fit matters, so follow-up visits fine-tune contacts and comfort.
On waking, your jaw feels sore until the splint comes out. For many with TMJ disorder, night wear reduces morning muscle fatigue and protects enamel. In disc displacement with reduction, anterior repositioning splints have shown benefits for joint noises and function compared with some other designs, when used for the right diagnosis [16]. When the joint is locked without reduction, some reviews find that procedures like arthrocentesis can yield larger gains in mouth opening than splints alone, which helps guide sequencing of care [17].
Daily use should follow a plan. Most patients start with nighttime wear, brief check-ins, and home strategies that limit jaw overload. Short-term daytime wear is sometimes added, but only for defined goals and under supervision. Your dentist will monitor comfort, tooth contacts, and range of motion, and will adjust or change the appliance as symptoms evolve. Splints are not a stand‑alone cure; they work best alongside habit coaching, exercises, and targeted therapy to match your specific findings [15]. Thoughtful follow-up keeps splint therapy safe and effective.
When to Seek Help for TMJ Disorder
Seek care if jaw pain, clicking with pain, or stiffness lasts more than a few days, or if chewing and speaking become difficult. Get prompt help for locking, sudden bite changes, swelling, or pain that wakes you at night. Urgent evaluation is also important after injury to the jaw or face, or when fever and spreading facial swelling are present.
During dinner, your jaw shifts and your bite suddenly feels off. New locking or a jaw that will not open or close smoothly can signal a disc or muscle problem that benefits from early management. Persistent morning soreness, chipped edges, or line-like cracks on teeth point to heavy clenching or grinding that strains the joint and muscles. Ear fullness, ringing, or headaches that seem tied to jaw use are also good reasons to be seen. Early assessment helps separate muscle-driven pain from joint issues and prevents small problems from becoming chronic.
If symptoms follow a hit to the chin, a wide yawn that “stuck,” or a dental procedure that required long opening, schedule an exam soon. Sudden swelling, fever, bad taste with swelling near the jaw, or trouble opening and swallowing can indicate infection or another condition that needs urgent care; review our guidance on what to do in a dental emergency if severe signs appear. For day-to-day problems, documenting when pain starts, which foods aggravate it, sleep quality, and any jaw sounds gives your clinician a clear starting point. Bring any mouthguard or splint you use so fit and wear patterns can be checked.
At the visit, your dentist will examine jaw motion, muscle tenderness, and bite contacts, then decide whether imaging or referral is needed. Many people improve with simple steps when started early, so do not wait for a flare to settle on its own if it keeps returning. Prompt evaluation supports stable, comfortable jaw function.
Lifestyle Changes for TMJ Relief
Daily habits can reduce jaw strain and ease pain. Key steps include relaxing the jaw during focused tasks, moderating chewing demands, and setting up sleep and posture to support the joints. With steady practice, many people notice fewer flares and smoother motion. These strategies complement care for TMJ disorder.
During emails, you catch yourself pressing your teeth together. Build short “unclench” cues into the day with a phone reminder or sticky note. Let your teeth rest slightly apart, with lips closed, whenever you are not eating. Keep your monitor at eye level, relax the shoulders, and hold the phone up rather than tucking it between your ear and shoulder. Skip chewing on ice, pens, or hard snacks, and avoid biting nails. Share chewing between both sides to spread load, and sip water through the day to prevent dry, tense muscles.
Sleep is another lever. Aim for side or back sleeping with your neck in a neutral position, using a pillow that neither tilts your chin up nor tucks it down. Try to keep yawns smaller and controlled, opening within a comfortable range instead of stretching wide. Limiting late caffeine and alcohol may reduce nighttime clenching for some people. A brief pre-sleep wind-down with quiet breathing and gentle facial relaxation helps many settle the jaw before bed.
Eating patterns matter when symptoms spike. Choose tender textures for a few days, cut food into small pieces, and slow your pace so each bite is easy. Avoid long chewing tasks like sticky candies or dense, crusty bread until the area calms. Plan brief “jaw breaks” during long meetings, driving, or workouts that tend to tighten your face and neck. Track what helps in a simple note on your phone, including activities, sleep quality, and how the jaw feels in the morning. Share that record at your visit so your clinician can target the next step.
Consistent, small adjustments often lower pain and keep flares short. Small, steady habit changes add up to calmer, more reliable jaw comfort.
Preventive Measures for TMJ Disorder
Prevention centers on limiting jaw overload, keeping motion comfortable, and noticing early warning signs. Practical steps include planning chewing tasks, avoiding extreme opening, and maintaining smooth, relaxed function during focused activities. Regular dental checkups can spot tooth wear or bite changes early, so small adjustments prevent bigger flares. These habits help many people avoid recurrent jaw pain and stiffness.
Before a recital, your jaw feels tight. Think “load management” for the joint: spread tough foods across days, not one meal; warm up with gentle, small-range opening before singing, heavy workouts, or long meetings; and avoid sudden, wide yawns. Musicians, public speakers, and athletes can rotate tasks, rest the jaw between sets, and keep the head centered over the torso rather than resting the chin on a hand. These small choices minimize peak forces that irritate joint tissues.
Dental prevention is equally important. Ask your clinician to check for scalloped tongue edges, line-like enamel cracks, or flat spots on teeth that signal heavy contact at night. Use well-fitted, supervised appliances if they are part of your plan, and be cautious with long-term wear of over‑the‑counter guards without follow-up. Evidence for irreversible bite changes as a preventive tactic is mixed, so routine occlusal adjustments are not advised purely to prevent symptoms [18].
Plan ahead for times when risk is higher. During pregnancy, TMD symptoms are more common in pooled studies, so gentle load management and early education can be especially helpful [19]. Wind‑instrument players, powerlifters, and folks with highly focused desk work can schedule brief jaw rests and vary tasks that tend to trigger bracing. If new medications, allergies, or sleep changes increase clenching or disturb rest, let your clinician know so your plan can be refined. Consistent habits support calm, durable jaw function.
Frequently Asked Questions
Here are quick answers to common questions people have about TMJ Disorder: Causes & Treatments in Glendale, AZ.
- What are the common symptoms of TMJ disorder?
Common symptoms of TMJ disorder include jaw pain near the ear or face, clicking or popping sounds when opening or closing the mouth, and difficulty opening the jaw wide. You might also experience headaches, neck pain, and unusual ear sensations like ringing or fullness. Some people notice their jaw shifts or locks, especially in the morning or after heavy use.
- How is TMJ disorder diagnosed?
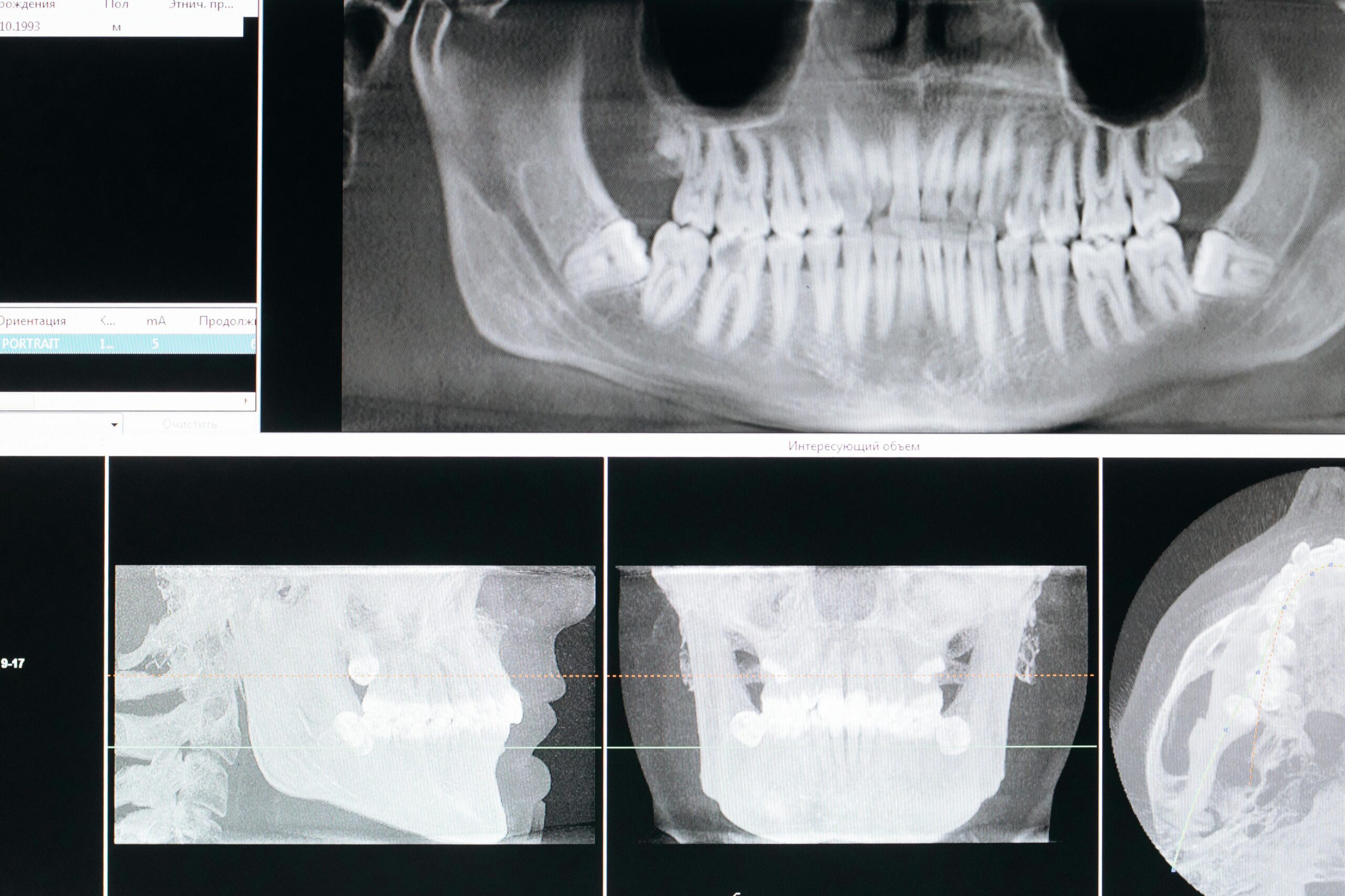
TMJ disorder is diagnosed through a combination of medical history reviews and a physical exam of the jaw. Your dentist will check jaw motion, listen for joint sounds, and assess any muscle tenderness. They might also ask about habits like teeth grinding or clenching, stress levels, and any changes in your bite. Imaging tests like X-rays may be used if there is a need to see the joint details more clearly.
- What causes TMJ disorder to flare up?
TMJ disorder flare-ups can be triggered by stress, repetitive jaw actions like chewing gum or teeth grinding, and poor posture. Changes in weather or sleep disturbances can also intensify symptoms. If you frequently experience flares, identifying personal triggers and modifying behavior can help reduce occurrences.
- Are there any simple exercises for TMJ pain relief?
Yes, several simple exercises may help relieve TMJ pain by promoting muscle relaxation and improving jaw function. Try gentle jaw stretches, like opening and closing your mouth slowly and repeatedly, or side-to-side movements with control. Consult with a healthcare provider for personalized exercises that suit your condition. Always ensure exercises do not cause more pain.
- How is a night guard used in TMJ treatment?
A night guard is a custom-fitted dental appliance that fits over your teeth to lessen the impact of teeth grinding or clenching, especially during sleep. It helps distribute pressure evenly across your jaw and reduces stress on the TMJ and surrounding muscles. While it’s most commonly worn at night, some people may also use it during high-stress periods or during the day if advised by their dentist.
- Can lifestyle changes help manage TMJ disorder?
Yes, lifestyle changes can significantly help manage TMJ disorder symptoms. Adjustments include eating softer foods, avoiding activities that stress the jaw like chewing gum, and practicing relaxation techniques to reduce stress. Improving posture and increasing hydration can also benefit jaw health. Consistent nighttime habits, such as using a supportive pillow and avoiding late stimulants, can decrease night-time clenching.
- How can I prevent TMJ disorder from worsening?
To prevent TMJ disorder from worsening, focus on avoiding overuse of the jaw. This includes limiting chewy and hard foods, refraining from excessive yawning or wide opening of the mouth, and maintaining proper jaw posture. Regularly visit your dentist for checkups to catch any early changes in your bite that might need addressing. Managing stress through relaxation practices can also prevent symptoms from escalating.
- Why does my jaw click or pop?
Jaw clicking or popping often occurs when the soft disc within your TMJ moves slightly out of place and then returns during motion such as opening and closing your mouth. If the clicking is painless and occasional, it may not be a significant concern. However, if it is accompanied by pain, limited jaw movement, or locking, it could indicate TMJ disorder requiring an evaluation.
References
- [1] Diving into discomfort: orofacial pain dynamic-A systematic review. (2025) — PubMed:40416680 / DOI: 10.3389/fpubh.2025.1553541
- [2] Global prevalence of temporomandibular disorders: a systematic review and meta-analysis. (2025) — PubMed:41070533 / DOI: 10.22514/jofph.2025.025
- [3] Anatomical Changes After Stabilisation Splint Therapy: A Systematic Review and Meta-analysis. (2025) — PubMed:40818265 / DOI: 10.1016/j.identj.2025.100952
- [4] Dry Needling in Treatment of Temporomandibular Joint Disorders: A Systematic Review. (2025) — PubMed:40917038 / DOI: 10.1002/cre2.70214
- [5] Headaches in dental practice: A narrative review of primary, secondary, and facial presentations. (2025) — PubMed:40908067 / DOI: 10.1016/j.adaj.2025.06.010
- [6] AWAKE BRUXISM PREVALENCE ACROSS POPULATIONS: A SYSTEMATIC REVIEW AND META-ANALYSIS. (2025) — PubMed:40716827 / DOI: 10.1016/j.jebdp.2025.102171
- [7] Imaging techniques for evaluating temporomandibular joint involvement in juvenile idiopathic arthritis: a systematic review. (2025) — PubMed:40992986 / DOI: 10.1016/j.oooo.2025.08.006
- [8] Association of temporomandibular disorders and other jaw anomalies in chewing gum users-a systematic review. (2025) — PubMed:41070532 / DOI: 10.22514/jofph.2025.022
- [9] Prevalence of temporomandibular disorder in irritable bowel syndrome (IBS) patients: a systematic review. (2025) — PubMed:41070534 / DOI: 10.22514/jofph.2025.026
- [10] Transforming TMJ pain relief: Hyaluronic acid’s efficacy in focus – a comprehensive systematic review and meta-analysis of randomized controlled trials. (2025) — PubMed:41201237 / DOI: 10.17219/dmp/194565
- [11] The effectiveness of physiotherapy for chronic headaches in patients with temporomandibular disorders: a systematic review. (2025) — PubMed:41064810 / DOI: 10.3389/fresc.2025.1647927
- [12] Controversies in the management of arthrocentesis treatment of temporomandibular joint disorders: systematic review. (2025) — PubMed:41020083 / DOI: 10.25122/jml-2024-0402
- [13] Effectiveness of treatments for temporomandibular joint osteoarthritis: a systematic review and meta-analysis. (2025) — PubMed:41091224 / DOI: 10.1007/s00784-025-06581-1
- [14] Autogenous Injections in Temporomandibular Disorders: A Systematic Review. (2025) — PubMed:41010846 / DOI: 10.3390/jcm14186640
- [15] Effectiveness of conservative therapeutic modalities for temporomandibular disorders-related pain: a systematic review. (2023) — PubMed:36354093 / DOI: 10.1080/00016357.2022.2138967
- [16] Effectiveness of anterior repositioning splint versus other occlusal splints in the management of temporomandibular joint disc displacement with reduction: A meta-analysis. (2024) — PubMed:38263554 / DOI: 10.4103/jips.jips_355_23
- [17] Arthrocentesis versus occlusal coverage splints in the management of disc displacement without reduction: a systematic review and meta-analysis. (2024) — PubMed:38702202 / DOI: 10.1016/j.ijom.2024.03.013
- [18] Occlusal interventions for managing temporomandibular disorders. (2024) — PubMed:39282765 / DOI: 10.1002/14651858.CD012850.pub2
- [19] Prevalence of temporomandibular disorders (TMD) in pregnancy: A systematic review with meta-analysis. (2023) — PubMed:37021601 / DOI: 10.1111/joor.13458