What Are the Early Oral Cancer Signs?
Early oral cancer signs often look like small changes in the mouth that do not go away. Watch for a sore that lasts longer than two weeks, a red or white patch that persists, or a firm area you can feel. Unexplained bleeding, numbness, or pain when swallowing can also be early clues. If something new lingers or worsens, it deserves an exam.
A small mouth sore lingers past two weeks despite saltwater rinses. Common early changes to notice include:
- A sore or ulcer that does not heal within 14 days.
- Red (erythroplakia), white (leukoplakia), or mixed red-white patches that persist.
- Unexplained bleeding, tingling, or numbness in the lips, tongue, or cheek.
- A firm lump, thickened area, crust, or rough surface on soft tissues.
- Painful swallowing, a feeling of something stuck, or persistent throat discomfort.
- A loose tooth or dentures that suddenly fit poorly without a clear cause.
- Ongoing hoarseness or one-sided ear pain without ear findings.
These changes often appear on the tongue edges, floor of the mouth, soft palate, or lips. Many early lesions are painless, which is why the “does not heal in two weeks” rule is useful. Because infections, trauma, and aphthous ulcers can mimic early cancer, a dentist’s visual and tactile exam is important. Visual screening with prompt referral helps find potentially malignant disorders earlier, including in low-resource settings [1]. Delays often come from patient and system barriers, so recognizing warning signs and seeking care quickly can shorten time to diagnosis [2]. If you use tobacco or drink heavily, be especially attentive to changes; learn more about smoking and oral health.
If a spot lasts beyond two weeks, grows, or returns, schedule an evaluation. Check our current hours and plan a visit for an exam and, if needed, a biopsy referral. While new tools like AI and salivary tests are being studied, they do not replace a careful clinical exam and follow-up [3]. Early attention can make a significant difference in outcomes.
Common Oral Cancer Symptoms to Watch For
Oral cancer symptoms often show up as changes in how your mouth works or feels. Watch for new problems chewing, moving your tongue, or opening wide, as well as a firm lump inside the mouth or in the neck. A non-healing extraction site that stays tender or raw, or speech that starts to sound different, can also be important clues. Persistent bad breath that is new and unexplained may accompany these changes.
These symptoms happen because growing lesions can irritate nerves and muscles, affect saliva flow, or spread to nearby lymph nodes. Limited jaw opening, called trismus, may develop when tissues of the cheek or jaw muscles are involved. You notice your jaw will not open as wide for a week. Tongue lesions can make certain sounds harder to form, leading to a new lisp or slurred words. A firm, painless swelling beneath the jawline or along the side of the neck can represent enlarged nodes that need evaluation. Because of this, a careful neck check is part of a complete oral exam.
Not every mouth change is cancer. Common conditions such as canker sores, gum disease, TMJ problems, or bite trauma can look or feel similar early on. The difference is that cancer-linked changes tend to persist, progress, or feel different from your usual patterns. If a spot, lump, or function change is new, one-sided, or steadily worsening, schedule a focused exam. Dentists assess the lips, cheeks, tongue, palate, and floor of mouth, and they also check the neck; when needed, they coordinate imaging or refer for a biopsy. Recognizing oral cancer signs early supports timely care and clearer next steps. Joint care between dental and medical teams helps sustain long-term wellness.
Identifying Mouth Cancer Signs Early
Early identification starts with noticing new, unusual changes and tracking whether they fade or progress. Look for differences in color, texture, or thickness, and note any area that feels different when your tongue moves across it. If a change persists or evolves, that is a cue to book a focused exam. Paying attention to subtle shifts helps you spot oral cancer signs sooner.
You feel a new rough patch under your tongue during brushing. In good light with clean hands, gently pull back your lips and cheeks, then look at the sides and underside of the tongue, the floor of mouth, and the palate. Compare both sides for symmetry, and lightly press tissues to check for firmness. A quick note in your phone, plus a clear photo from the same angle a few days apart, can help you track trends. People with tobacco or heavy alcohol exposure, prior oral lesions, or HPV risk may benefit from more frequent self-checks. Small, persistent changes deserve a professional look, even if they do not hurt.
Dental teams use a methodical visual and tactile exam to evaluate suspicious areas and decide on next steps. When appropriate, brush-based cytology can help triage lesions by providing cell-level information with useful accuracy for early detection of potentially malignant disorders [4]. Image analysis with smartphones and digital cameras is also being studied and shows promise for detecting concerning features earlier in accessible settings [5]. Some clinics use additional risk markers, such as DNA ploidy, to help flag lesions with higher malignant potential [6]. Research on salivary cytokines may further support diagnosis and prognosis in the future, though these tests are not yet routine in general practice [7]. Regular dentist visits, including thorough exams during routine cleaning visits, create more chances to catch small shifts early.
If you observe a change that keeps returning, enlarges, or interferes with speaking or eating, schedule an evaluation. Coordinated care often leads to clearer plans and calmer days.
Understanding Leukoplakia and Oral Cancer
Leukoplakia is a white patch in the mouth that cannot be wiped off and is not explained by another condition. It is classified as an oral potentially malignant disorder, which means some lesions can turn into cancer over time. Most leukoplakias do not become cancer, but certain patterns carry higher risk and deserve close follow-up. Knowing how it relates to oral cancer signs helps you act early and appropriately.
Risk is not the same for every white patch. Non-homogeneous, speckled, or thickened lesions are more concerning than thin, uniform ones. A specific subtype, proliferative verrucous leukoplakia, has a particularly high chance of malignant change and needs specialist monitoring and timely treatment [8]. Oral potentially malignant disorders, including leukoplakia, occur worldwide and contribute meaningfully to the pool of cancers diagnosed in the mouth [9]. Although less common, these lesions can also appear in younger people, so age alone should not delay evaluation [10].
Evaluation starts with a careful exam to rule out look-alikes, such as frictional keratosis or fungal plaques. If a lesion persists or shows worrisome features, a biopsy confirms the diagnosis and guides care. Management often includes removing irritants like tobacco, improving oral hygiene, and setting a surveillance schedule. In selected cases, treatments such as surgical or laser removal, and even photodynamic therapy, can reduce lesion burden when used appropriately under specialist care [11]. These steps help lower risk while preserving function and comfort.
You notice a chalky patch on the inside of your cheek. If a white area persists, thickens, or feels firmer over time, plan an exam rather than waiting for it to fade. Early documentation with a clear photo and prompt assessment make trends easier to judge. When concerns arise, collaboration between your dentist and specialists provides a clearer plan and steadier follow-up. Early attention often changes the course and calms uncertainty.
Recognizing Red Patches in the Mouth
Red patches in the mouth are areas of bright to dark red tissue that stand out from surrounding pink mucosa. Many are caused by irritation or infection and fade with time, but a flat, velvety red area that lingers or bleeds easily should be checked. Because certain persistent red lesions can signal disease, recognizing their features helps you decide when to schedule an exam.
Color comes from increased visibility of blood vessels near the surface when the protective top layer thins. Simple causes include bite or denture friction, hot-food burns, or fungal overgrowth. These usually improve as the tissue heals or the irritant is removed. In contrast, a concerning red patch, often called erythroplakia, tends to look uniformly red, well defined, and smooth or velvety. It may appear on the side of the tongue, floor of the mouth, or soft palate, and may bleed with light brushing. Noting these details can help your dentist assess risk and decide next steps.
You notice a bright red spot that bleeds when floss touches it. Give minor injuries time to settle, keep the area clean, and avoid spicy foods or alcohol-based rinses that sting. If the red area keeps returning, enlarges, develops a tender or firm feel, or starts to affect speech or swallowing, plan a focused evaluation. Take a clear photo and record the date, which makes changes easier to track over days and weeks. In people with tobacco or heavy alcohol exposure, a persistent red patch deserves particular attention as part of monitoring for oral cancer signs.
During a visit, your dentist will measure the patch, compare both sides of the mouth, and gently feel for firmness or nearby lymph node swelling. The team will look for obvious irritants, treat any infection, and decide whether short-term review or a biopsy referral is appropriate. Early evaluation can clarify the cause, reduce worry, and guide timely care. Prompt attention often leads to simpler, more effective treatment plans.
The Importance of Oral Screening
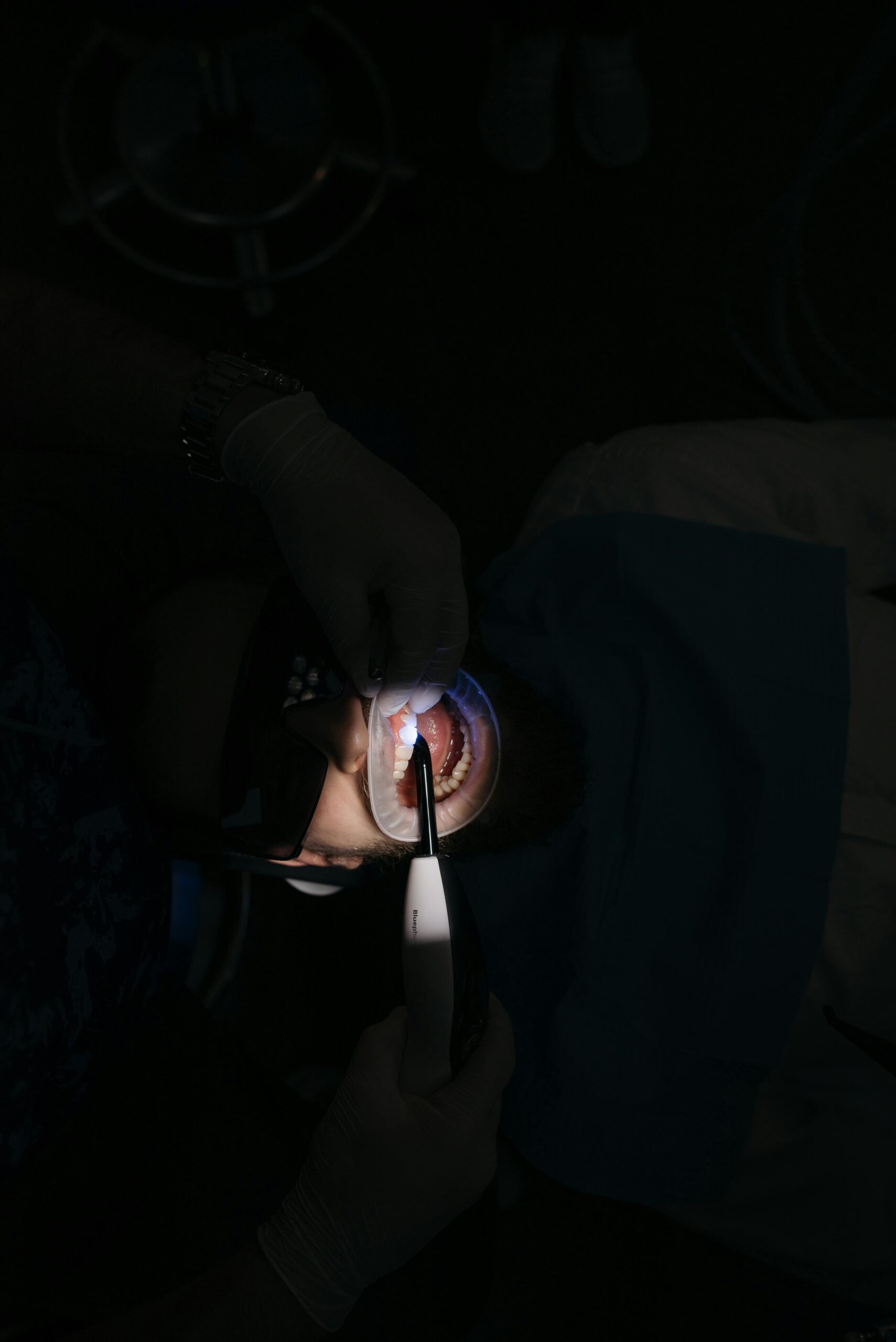
Oral screening helps catch small, silent changes before they become harder to treat. A quick visual and tactile exam can reveal early oral cancer signs, as well as other conditions that mimic them. Screening is painless, takes only a few minutes, and is part of a complete head and neck check.
Most early mouth lesions do not hurt, so waiting for pain can delay care. During screening, your dentist reviews risk factors, examines the lips, cheeks, tongue, floor of mouth, palate, and gently palpates the neck. Clear documentation and short-term follow-up make it easier to see trends if a spot changes. Finding disease earlier often means less extensive treatment and better function afterward. During a checkup, a dentist spots a tiny red patch you missed.
Screening is not a one-time event. It works best when it happens at routine dental exams, because small shifts are easier to track on a regular cadence. If you use tobacco, drink heavily, have past oral lesions, or other risks, your dentist may suggest shorter intervals. When a finding appears, the plan may include removing irritants, re-evaluating soon, or referring for imaging or biopsy. If specialists are needed, your dental team can coordinate with oral surgery or ENT so next steps are clear. If you are building consistent care, see our guide to finding a nearby dentist. Coordinated care often leads to clearer days and calmer nights.
How HPV Relates to Oral Cancer
Human papillomavirus (HPV) is a common virus that strongly relates to cancers of the oropharynx, especially the tonsils and base of tongue. In the mouth itself, HPV’s role is weaker than tobacco and alcohol, but it can contribute in some cases. Understanding this link helps you focus on throat-centered changes, not just visible mouth sores, when watching for oral cancer signs.
HPV spreads through close intimate contact. Most oral HPV infections clear on their own, but a small portion persist. Studies show oral HPV can be found in healthy people as well as those with lesions, and rates differ by region and risk factors [12]. HPV-related throat cancers often present with symptoms deeper in the throat rather than a surface spot you can see. You notice a lingering sore throat and a new neck bump. These cancers also show different patterns over time and survival compared with non-HPV tumors, which is why doctors consider HPV status when planning care [13].
Here is what that means for you. Mouth sores that do not heal still matter, but HPV-related disease may appear as trouble swallowing, a persistent throat ache, voice changes, one-sided ear discomfort, or a firm neck swelling. If symptoms cluster in the throat or neck and do not fade, schedule an exam. Your dentist and medical team can evaluate the mouth, tonsils, and neck, and coordinate imaging or referral when needed. HPV vaccination and healthy habits reduce risk over time, but they do not replace attention to new, persistent changes. Early evaluation brings clarity and a faster path to the right next step.
Coordinated care helps keep small findings from becoming bigger problems.
When to Seek Professional Evaluation
Schedule an exam if a mouth change lasts longer than two weeks, grows, bleeds, or feels unusually firm. Seek prompt care for a new neck lump, trouble swallowing, limited jaw opening, numbness, or a persistent one-sided earache. If a spot returns after healing or keeps changing, it merits a professional look. A lower lip sore persists despite avoiding spicy foods for two weeks.
Timing matters because many early lesions are painless and subtle, yet easier to treat when found small. Simple irritation usually improves once the cause is removed, while concerning areas tend to persist or progress. A dentist’s exam includes careful inspection and gentle palpation to judge texture, borders, and nearby lymph nodes. If features are suspicious, a biopsy confirms the diagnosis and guides next steps.
Certain situations call for an earlier visit. People who use tobacco, drink heavily, are immunosuppressed, or who have had head and neck cancer should not wait if a new change appears. Combining risks increases concern, so persistent red, white, or mixed-color patches deserve timely evaluation. Before your appointment, note when you first saw the change, take a clear photo in the same lighting, and write down any symptoms like pain with swallowing or voice change. These details help your clinician compare findings over time.
Here is a simple approach. If a spot is new and fades within days, keep the area clean and watch it. If it lingers beyond two weeks, enlarges, or affects speaking or eating, book an exam. Rapidly worsening symptoms, such as difficulty swallowing liquids or breathing, need urgent medical attention. Recognizing oral cancer signs early helps you take the right step at the right time. Early evaluation often means a simpler path forward.
Symptoms That Require Immediate Attention
Some mouth and throat symptoms should be checked right away. Seek urgent care for trouble breathing, choking on liquids, or bleeding that does not stop with gentle pressure. A quickly enlarging lump in the mouth or neck, new numbness of the lip, chin, or tongue, or a jaw that suddenly will not open also need prompt evaluation. Sudden, severe pain with fever or rapidly worsening swelling is another warning.
These signs matter because fast changes can reflect deeper tissue involvement or spread to nearby lymph nodes. Tumors can press on nerves and cause numbness or weakness, while fragile, abnormal surface tissue may bleed easily. A new, hard neck lump appears after a week of sore throat. Limited jaw opening, called trismus, can point to disease affecting the chewing muscles or spaces around the jaw. When symptoms escalate quickly, timely assessment helps protect breathing, swallowing, and speech.
Until you are seen, keep the area clean and avoid irritants like alcohol-based rinses or very spicy foods. If bleeding occurs, apply gentle, steady pressure with clean gauze for several minutes. Do not wait for symptoms like tongue weakness, voice changes, or one-sided ear pain with a firm neck swelling to fade on their own. If you are unsure whether to wait or act now, see our overview of urgent steps in dental emergencies.
At the visit, your clinician will check the mouth, throat, and neck, assess airway safety, and decide on imaging or a biopsy referral. Bring notes on when the problem began, what has changed, and any photos that show progression. Some oral cancer signs are subtle, but the red flags above call for prompt attention. Prompt evaluation supports better outcomes and preserves function.
Risk Factors for Developing Oral Cancer
Several factors raise the chance of oral cancer. The biggest are tobacco in any form and heavy alcohol use. Other risks include betel quid or areca nut chewing, long-term sun exposure to the lips, certain viral and immune conditions, and prior mouth lesions. Knowing your risk helps you interpret oral cancer signs sooner.
Smoking bathes mouth tissues in carcinogens, while alcohol can make these substances penetrate more easily and form acetaldehyde, a toxic byproduct. Smokeless tobacco and areca nut products repeatedly irritate tissues and expose cells to carcinogens. In some regions, opium use has also been linked to higher rates of oral cancer [14]. A person chews betel quid at social events for years. Reducing or stopping these exposures can lower risk over time.
Sunlight is a key risk for cancers of the lower lip, so consistent shade and SPF lip protection matter. HPV plays a larger role in throat cancers than in the mouth, but it can contribute in selected cases. People with weakened immunity, prior head and neck cancer, or a strong family pattern may need closer follow-up. Recent reviews also describe changing patterns, including oral tongue cancer in females [15]. Emerging research shows that DNA methylation, an epigenetic marker, is associated with oral cancer risk, which may help explain individual differences in susceptibility [16].
Some risks are modifiable, and others are not. Your dental team can review your history, then tailor screening intervals and self-check guidance to your profile. If you carry multiple risks, check your mouth between visits and schedule promptly if a change persists. Thoughtful attention to risk helps you act early and confidently.
Maintaining Oral Health for Prevention
Prevention focuses on protecting mouth tissues, reducing irritants, and keeping a routine that makes changes easy to spot. Good daily care, a balanced diet, and regular dental exams help your mouth heal quickly and highlight new concerns. These steps reduce common triggers and make it easier to notice oral cancer signs early.
Start with consistent home care. Brush gently twice a day with a soft brush, clean between teeth daily, and stay well hydrated so saliva can protect tissues. Choose alcohol-free rinses if your mouth feels dry or easily irritated. For step-by-step home routines, see our practical hygiene tips.
Reduce exposures that inflame or injure the lining of your mouth. Avoid tobacco in any form, and limit alcohol, which can compound tissue irritation. Use a brimmed hat or SPF lip balm to protect the lower lip from sun. Make sure dentures and retainers fit smoothly, and have sharp tooth edges or broken fillings polished or repaired to prevent chronic rubbing.
Support tissue resilience. Drink water regularly, and ask about dry mouth strategies if medicines reduce saliva. Eat a variety of fruits, vegetables, and lean proteins to provide nutrients that aid repair. You notice your lips feel burned after a day outdoors. Small notes and clear photos of any spot that lingers help you and your dentist judge change over time.
Routine dental visits add professional screening and documentation to your self-care. Your team can remove plaque and calculus, check soft tissues and lymph nodes, and advise on habits tailored to your risks. These steady habits build a healthy baseline so new changes stand out and get checked promptly. Early, steady habits protect your mouth for the long run.
Tips for Regular Self-Exams
Self-exams help you spot small changes before they become problems. Check monthly under bright light, with clean hands, and note anything new that does not fade between checks. These steady habits make oral cancer signs easier to notice early.
Start with prep. Remove dentures or retainers. Use a small flashlight and a hand mirror. A clean tissue or gauze helps you gently hold and move your tongue. You catch a subtle red area while drying your tongue with gauze.
Look methodically so you do not miss areas. Examine the lips, then cheeks by pulling them away and turning your head to change the angle. Check the gums and the roof of the mouth. Lift the tongue to view the floor of the mouth, then look at the top, sides, and underside of the tongue. Feel with clean fingers for any firm area or tender spot, and compare left to right for symmetry. Avoid scraping or picking, which can irritate tissue and hide useful details.
Include a quick neck check. With gentle pressure, feel under the jaw and along the sides of the neck for any firm, painless swelling. If you find something new, make a simple record. Take a clear photo in the same lighting and add a short note about color, size, and feel. At the next self-check, compare photos to see if the area is settling or changing.
Build the exam into routines you already have. Many people pair it with evening brushing. If you want a refresher on comfortable brushing positions and lighting, see our guide on brushing technique. This pairing keeps the process brief and consistent.
What happens next matters. If a spot keeps returning, slowly enlarges, becomes firmer, or starts to affect speaking or swallowing, schedule a focused exam. Save your notes and photos; they help your dentist understand the timeline and decide on imaging or a biopsy referral when appropriate. Simple, repeatable self-checks make professional evaluations clearer and faster. Prompt attention supports long-term oral health and peace of mind.
Frequently Asked Questions
Here are quick answers to common questions people have about Oral Cancer Signs & Symptoms in Glendale, AZ.
- What are some common early signs of oral cancer?
Common early signs of oral cancer include a sore or ulcer that doesn’t heal within two weeks, red or white patches in the mouth, and unexplained bleeding or numbness. Other signs can be lumps or thickened areas, painful swallowing, or a persistent sore throat. These changes often appear on the lips, tongue edges, or floor of the mouth. Not every change means cancer, but persistent issues deserve a dentist’s attention to rule out potential problems.
- How do I perform a self-exam for mouth cancer?
To perform a self-exam, use a bright light and mirror. Check your lips, cheeks, gums, tongue, and throat systematically for unusual changes like lumps, spots, or persistent sore areas. Gently feel your neck for any firm or painless lumps. If you notice anything new that persists for more than a couple of weeks, make notes and take photos to track changes. Schedule a dentist visit if any area does not heal or worsens.
- What should I do if I find a persistent red or white patch in my mouth?
If you discover a red or white patch that does not go away within two weeks, consider scheduling an exam with your dentist. Persistent patches can indicate underlying issues that need professional evaluation. During the appointment, your dentist will check the patch’s characteristics and determine if further tests, like a biopsy, are necessary. Keeping a photo log of changes can provide useful information for the assessment.
- Can lifestyle choices affect my risk of oral cancer?
Yes, lifestyle choices play a significant role in your risk of developing oral cancer. Tobacco use and heavy alcohol consumption are major risk factors. Other factors include frequent sun exposure to the lips, consuming betel quid or areca nut, and having a weakened immune system. Making healthier choices, like quitting smoking and reducing alcohol intake, can help lower your risk. Regular dental checkups are also important for early detection.
- Why is regular screening important for oral health?
Regular oral health screenings help catch small issues before they develop into serious problems. A comprehensive examination by your dentist can reveal early signs of oral cancer and other conditions. Screening is painless, quick, and typically part of your routine dental care. It allows for early intervention, potentially leading to better treatment outcomes and preserving your oral functions over time.
- What should I do if I experience symptoms that require urgent dental attention?
If you experience symptoms like trouble breathing, uncontrollable bleeding, or a quickly enlarging lump in your mouth or neck, seek urgent care immediately. These symptoms could indicate more serious issues requiring prompt evaluation. Until you are seen, keep the affected area clean and avoid potential irritants like alcohol-based mouthwashes. If in doubt, consult with healthcare professionals to assess the urgency of your symptoms.
References
- [1] Screening Tools and Strategies for Early Detection of Oral Cancer and Potentially Malignant Disorders in Rural and Low-Resource Populations: A Systematic Review. (2025) — PubMed:41285247 / DOI: 10.1016/j.jormas.2025.102667
- [2] Patient and System Barriers to Early Diagnosis of Oral Cancer in the UK. (2025) — PubMed:41240321 / DOI: 10.1111/odi.70125
- [3] AI MAY SHOW COMPARABLE DIAGNOSTIC ACCURACY TO EXPERTS IN ORAL CANCER DETECTION, BUT EVIDENCE REMAINS LIMITED AND OF LOW CERTAINTY. (2025) — PubMed:41290266 / DOI: 10.1016/j.jebdp.2025.102199
- [4] Accuracy of Cytological Methods in Early Detection of Oral Squamous Cell Carcinoma and Potentially Malignant Disorders: A Systematic Review and Meta-Analysis. (2025) — PubMed:40589386 / DOI: 10.1111/jop.70010
- [5] Deep learning for early diagnosis of oral cancer via smartphone and DSLR image analysis: a systematic review. (2024) — PubMed:39587051 / DOI: 10.1080/17434440.2024.2434732
- [6] Diagnostic Accuracy of DNA Ploidy for Oral Potentially Malignant Disorders: A Systematic Review and Meta Analysis. (2025) — PubMed:40302066 / DOI: 10.31557/APJCP.2025.26.4.1155
- [7] Salivary cytokines as a biomarker for diagnosis, prognosis and treatment of oral squamous cell carcinoma: A systematic review. (2025) — PubMed:40243118 / DOI: 10.17219/dmp/186664
- [8] Malignant transformation of proliferative Verrucous Leukoplakia-systematic review & meta-analysis. (2025) — PubMed:39893387 / DOI: 10.1186/s12903-025-05565-7
- [9] Prevalence of oral potentially malignant disorders: A systematic review and meta-analysis. (2018) — PubMed:29738071 / DOI: 10.1111/jop.12726
- [10] Oral leukoplakia and erythroplakia in young patients: a systematic review. (2021) — PubMed:33187936 / DOI: 10.1016/j.oooo.2020.09.002
- [11] CLINICAL EFFICACY OF PHOTODYNAMIC THERAPY IN MANAGEMENT OF ORAL POTENTIALLY MALIGNANT DISORDERS: A SYSTEMATIC REVIEW AND META-ANALYSIS. (2024) — PubMed:38821659 / DOI: 10.1016/j.jebdp.2023.101899
- [12] Prevalence of oral HPV in healthy and lesion-bearing populations in Iran: a systematic review and meta-analysis. (2025) — PubMed:40346604 / DOI: 10.1186/s12903-025-06085-0
- [13] The epidemiological trends and survival of HPV-related oropharyngeal cancer other than tonsils and base of tongue – a systematic review and meta-analysis. (2025) — PubMed:40286702 / DOI: 10.1016/j.oraloncology.2025.107311
- [14] Opium use and oral cancer in Iran: A systematic review and meta-analysis. (2025) — PubMed:41029094 / DOI: 10.1097/MD.0000000000044765
- [15] Epidemiological trends and characteristics of oral tongue cancer in females: systematic review and meta-analysis. (2025) — PubMed:41298213 / DOI: 10.1016/j.ijom.2025.10.013
- [16] ASSOCIATION OF DNA METHYLATION AND ORAL CANCER RISK: A SYSTEMATIC REVIEW AND META-ANALYSIS. (2025) — PubMed:41290267 / DOI: 10.1016/j.jebdp.2025.102169